The Regional Anesthesiology and Acute Pain Fellowship at WashU Medicine offers multidisciplinary training at one of the nation’s consistently ranking top-10 leading academic medical centers.
The 12-month program is committed to preparing future leaders in regional anesthesia to start and lead an acute pain service after program completion. Fellows work clinically four days per week with one day dedicated to non-clinical, academic, or optional moonlighting activities. Clinical work is comprised of both inpatient and outpatient regional anesthesia as well as dedicated time on the acute pain service. Fellows also have the option to spend time supervising CRNAs as general anesthesiologists, but this – or performance of general anesthesia – is not required.
Recent graduates have performed over 1,500 ultrasound-guided procedures as well as thoracic epidurals and spinals. They learn how to place and manage both inpatient and outpatient peripheral nerve catheters. Under the direction of fellowship-trained physicians, fellows will spend eight weeks leading the acute pain service at WashU, learn how to manage pain with state-of-the-art multimodal techniques, and mentor resident anesthesiologists. International rotations are available. A new 2-week rotation has been approved for the Amsterdam University Medical Center. Previous fellows have rotated in Ghana, The Philippines, and Guatemala.
By the end of the fellowship, graduates will be experienced in nearly all commonly performed regional anesthetics including, but not limited to, scalp blocks for craniotomy, interscalene, supraclavicular, infraclavicular and axillary brachial plexus blocks, forearm/wrist blocks, paravertebral, erector spinae, parasternal for cardiac surgery, epidural, spinal, PECS, serratus anterior, all TAP approaches, rectus sheath, suprainguinal fascia iliaca, femoral, sub gluteal sciatic, popliteal, iPACK, adductor canal, genicular, and ankle blocks. All fellows also have the opportunity to learn Point of Care Ultrasonography if desired.
Didactic education is primarily based on the flipped classroom model with faculty-led PBLs. Fellow-specific lectures also include medical economics and oral board review. Additionally, fellows participate in a quality improvement or research project. The regional and pain divisions within the department have multiple ongoing clinical QI and research projects available for fellows. Applicants also have the option of leading their own project. Alternatively, fellows can elect to participate in ongoing basic science research with our world-famous pain researchers. Accommodations can be made for MD/PhDs or experienced researchers. The Department of Anesthesiology at WashU is heavily funded by grants and consistently ranks among the top five nationally in NIH funding.
- Develop expertise in the practice and theory of regional anesthesia.
- Attain an expert-level proficiency in all commonly performed peripheral, truncal and neuraxial blocks.
- Assessment of anesthesia needs and options for patients having procedures in the ambulatory setting; develop anesthesia plan with necessary interventions to minimize risk.
- Medical evaluation of patients from history and physical examination to determine anesthesia risks; establish benefits of regional anesthesia.
- Understanding the medical benefits and advantages of regional anesthesia.
- Recommendations and consultation in perioperative pain management, evaluation of regional anesthetic intervention in the management of acute postoperative pain.
- Develop the techniques of regional anesthesia including understanding the specifics of anatomy involved in the performance of paravertebral blocks.
- Application and supervision of appropriate treatment protocols.
- Participate in research projects, presentations and teaching.
Fellows are encouraged to take advantage of numerous research opportunities available either within the Department of Anesthesiology or in collaboration with other departments in the Medical Center. This may include attainment of a Master’s in Clinical Investigation during the fellowship.
We participate in the San Francisco Match’s Central Application Service. To apply for our Regional Anesthesia and Acute Pain Fellowship, please visit their website to begin your application. We request the following supplemental documents as part of the SF match application:
- Curriculum Vitae
- Personal statement expressing your interest in the field of regional anesthesia
- USMLE scores
- ABA Board Scores (if available)
- 3 letters of recommendation written within the past year (preferably one from your residency director)
Supplemental documents should be sent to:
Lisa Parks
Regional Anesthesia and Acute Pain Fellowship
MSC 8054-92-2850
Training Locations
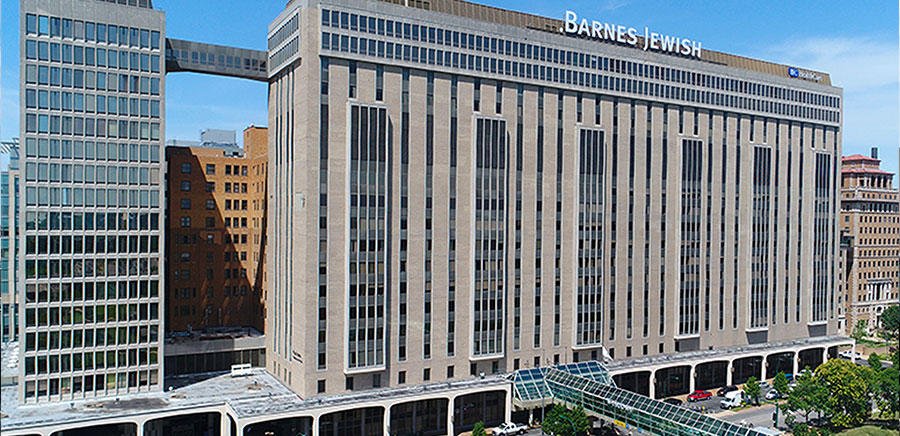
Barnes-Jewish Hospital
Barnes-Jewish Hospital is a Level 1 Trauma Center with 1,100 beds and an attached outpatient surgery center. BJH currently has 80 operating rooms.

Barnes-Jewish West County Hospital
A fast-paced private practice environment with 14 operating rooms. Regional anesthesia is primarily performed for orthopedic surgery at this site, including joint replacement and spine surgery. Individual fellows have performed over 30 ultrasound-guided blocks at this site in a single day.

Washington University and
Barnes-Jewish Orthopedic Center
A fast-paced private practice outpatient orthopedic surgery center with five operating rooms. Individual fellows have performed over 30 ultrasound-guided blocks at this site in a single day.
